Podcast 123: Exploring the Future of Health Care Delivery with Dr. Elliott Fisher

Summary
We wrap up Season 4 of Health Care Rounds with Dr. Elliott S. Fisher, former professor to our host, John Marchica, and well-known director of the Dartmouth Institute for Health Policy & Clinical Practice. Dr. Fisher gives us an in depth look at his recent paper, “The Single System Solution: How Competition Can Improve Care and Lower Costs.” Fisher talks about the three underlying causes of poor performance in our health system — flawed assumptions; inadequate information; and fragmented delivery, payment, and insurance systems — and how to address these issues through the implementation of a single health care system.
In this episode
Elliott S. Fisher, M.D., M.P.H.
 Elliott S. Fisher, M.D., M.P.H., is director of the Dartmouth Institute for Health Policy & Clinical Practice and Professor of Medicine, Community and Family Medicine and Health Policy at Dartmouth University’s Geisel School of Medicine. As a recognized leading health care researcher and advocate for improving health system performance, Dr. Fisher previously contributed to the concept of the “accountable care organizations” (ACOs) and has influenced research within the development of the Affordable Care Act.
Elliott S. Fisher, M.D., M.P.H., is director of the Dartmouth Institute for Health Policy & Clinical Practice and Professor of Medicine, Community and Family Medicine and Health Policy at Dartmouth University’s Geisel School of Medicine. As a recognized leading health care researcher and advocate for improving health system performance, Dr. Fisher previously contributed to the concept of the “accountable care organizations” (ACOs) and has influenced research within the development of the Affordable Care Act.
His research areas of expertise focus on Medicare, payment reform, and community health with an overall goal to deliver health care value. In his recent article, he focuses on the exploration of elements to success in health care reformation. Dr. Fisher is a well-known supporter of locally organized and operated community health collaboratives, leading to his role as co-founder of ReThink Health, an initiative designed to employ transformative change in order to deliver an improved well-being for all. Dr. Fisher earned his BA from Harvard College, his MD from Harvard Medical School, and his MPH from the University of Washington, now serving as a member of the Institute of Medicine of the National Academy of Sciences.
John Marchica
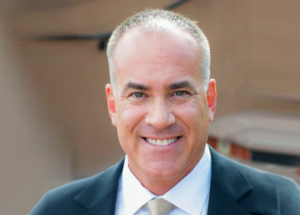 John Marchica is a veteran health care strategist and CEO of Darwin Research Group, a health care market intelligence firm specializing in health care delivery systems. He’s a two-time health care entrepreneur, and his first company, FaxWatch, was listed twice on the Inc. 500 list of fastest growing American companies. John is the author of The Accountable Organization and has advised senior management on strategy and organizational change for more than a decade.
John Marchica is a veteran health care strategist and CEO of Darwin Research Group, a health care market intelligence firm specializing in health care delivery systems. He’s a two-time health care entrepreneur, and his first company, FaxWatch, was listed twice on the Inc. 500 list of fastest growing American companies. John is the author of The Accountable Organization and has advised senior management on strategy and organizational change for more than a decade.
John did his undergraduate work in economics at Knox College, has an MBA and M.A. in public policy from the University of Chicago, and completed his Ph.D. coursework at The Dartmouth Institute. He is a faculty associate in the W.P. Carey School of Business and the College of Health Solutions at Arizona State University, and is an active member of the American College of Healthcare Executives.
Episode Transcript
Podcast 123: Exploring the Future of Health Care Delivery with Dr. Elliott Fisher
John Marchica:
Welcome to season four of Health Care Rounds. Here, we explore the vast and rapidly evolving health care ecosystem with leaders across the spectrum of health care delivery. Our goal is to promote ideas that advance the quadruple aim, including improving the patient experience, improving the health of populations, lowering the cost of care, and attaining joy in work.
I’m John Marchica, host of Health Care Rounds. I’m also the CEO of Darwin Research Group and faculty associate at the Arizona State University College of Health Solutions. Please don’t forget to rate and review us wherever you get your podcast, and send your questions, comments, or ideas for Health Care Rounds to podcast@darwinresearch.com. Let’s get started.
Kim Asciutto:
In this episode, John speaks to Dr. Elliott Fisher, Director of the Dartmouth Institute for Health Policy and Clinical Practice, and professor of medicine, community and family medicine and health policy at Dartmouth University’s Geisel School of Medicine. As a recognized leading healthcare researcher and advocate for improving health system performance, Dr. Fisher previously contributed to the concept of the accountable care organizations, and has influenced research within the development of the Affordable Care Act.
His research areas of expertise focus on Medicare, payment reform, and community health with an overall goal to delivery healthcare value. In his recent article, he focuses on the exploration of elements to success and healthcare reformation. Dr. Fisher is a well-known supporter of locally organized and operated community health collaboratives leading to his role as a co-founder of Rethink Health, an initiative designed to employ transformative change in order to deliver and improve wellbeing for all. Dr. Fisher earned his BA from Harvard College, his MD from Harvard Medical School, and his MPH from the University of Washington, now serving as a member of the Institute of Medicine of the National Academy of Sciences.
If you’re interested in Dr. Fisher’s recent paper talked about in this episode, please contact Dr. Fisher directly at elliott.s.fisher@dartmouth.edu.
John Marchica:
So, well, thank you, after so many fits and starts, Elliott, for taking some time to talk today. I think that folks are going to get a real kick out of this. I don’t know exactly who listens, but I have a general idea based on some comments that I tend to get from people. So, this is terrific. So, thank you.
Dr. Elliott Fisher:
Well, it’s a treat to be here.
John Marchica:
So, we’re going to get this, which is brilliant, and which I wish that I wrote because it all made so much sense to me.
Dr. Elliott Fisher:
You’re sweet.
John Marchica:
So, we’ll get to it, but the one question that I wanted to ask you as someone who is so seminal in the development of the ACO model, right? I think your definition at a MedPAC conference is quoted in about 300 papers, if not more, so probably 3,000 papers, but just looking back, how would you assess the performance of this model? I know there’s a lot of ways you can look at it, “Are you driving quality in the right direction? Have you saved money?” Thinking back that ’05 to ’07 timeframe when you had a set of expectations, how has the, and I guess in particular the Medicare, the various ACO models performed?
Dr. Elliott Fisher:
Well, I think it’s really a glass half full and a glass half empty. On the glass half full side, we have a thousand organizations that have become ACOs. In the estimate from 2019, we have 40 million Americans now covered under this model. So, there’s a lot of willingness on the part of providers to try new ways of working that encourage them to be integrated, that reward them for improving quality, and slowing cost growth.
The early evidence is that they’re having pretty substantial impact on quality, that they’re able to drive gains and quality, which we haven’t seen from most other models, right? Pay-per-performance in its general forms other than perhaps the readmission penalty, which really does seem to have had changed behavior. On most pay-per-performance programs based on quality, measures didn’t change much.
So, good evidence that it’s improving quality, and the cost savings are modest. They’re there. If you look at my [inaudible 00:05:10] work uses more meaningful counterfactuals than the Medicare benchmarks, which are biased in a number of ways. He’s estimating real and meaningful savings.
So, I think they’re slightly bending the cost for those people who are in the ACOs. When you look back, maybe it’s 1% or 2% against trend, which when you look back at our original paper that we did to try to persuade the CBO to do this, we estimated the ACO model could save between 0.5% and 1% of their investment. So, well, we’re at target. So, that’s that glass half full side.
I think the disappointment is, gosh, why hasn’t it really taken off, and why hasn’t it achieved greater savings? I think we really need to really look at how the model is operating in the context of US healthcare system within the rest of the payment models that are being used, mostly fee-for-service.
So, the most recent data on fee-for-service revenues is that, still, 87% of physicians are getting fee-for-service revenue. There are these still outliers like Kaiser Permanente, where people are capitated and on salary and the VA, but most physicians are receiving fee-for-service revenues.
70% of physician revenue remains purely from fee-for-service. Even inside ACOs, among physicians who are members of an ACO, 60% of their income is from fee-for-service. So, the challenge, perhaps the explanation, and I believe this is likely, the explanation is that in a system with fragmented incentives, it’s very hard to change behavior, especially when the dominant payment model is fee-for-service.
A wonderful paper in Health Affairs by folks from Harvard showed that you need to hit about over 60% of revenue from capitation to change the way you work, to start the innovations in care, to be able to do team-based care, to hire those people who can work in different ways to deliver great care to a panel of patients.
So, I think the reason that the ACO model has achieved less than we hoped is that we haven’t achieved the alignment toward that payment model. When McClellan and I laid out this vision in the paper that he was the first author on about a national strategy, it was about getting all payers to adopt this payment model, but I think the missing piece is alignment of payment models around global payment.
John Marchica:
Well, we’re going to get to that. I don’t want you to steal because you’re going to steal your own thunder.
Dr. Elliott Fisher:
No, I won’t. I’m just saying that’s why I’m disappointed.
John Marchica:
Yeah. It’s one of those things that we’ve been tracking here in the private sector. For a while there, we were tracking commercial ACO contracts. It seemed like back in 2012, 2013, 2014, whenever something new was coming out, then everyone would issue a press release. So, it was easy to track who was doing what, where. Now, in followup interviews, a lot of those early agreements have gone by the wayside, so it’s hard to know exactly how frequently or exactly to know whether those early agreements are still in place.
So, your paper, Reforming Healthcare, the single system solution, as I said, it’s terrific. I recommend that people who, hopefully, if they can get this paper, maybe they have to subscribe to the Catalyst.
Dr. Elliott Fisher:
They’ll let you pay for one copy.
John Marchica:
That’s nice of them.
Dr. Elliott Fisher:
That was my biggest mistake in the last five years was having this paper end up behind the paywall. Anyway, maybe that’s not quite the biggest mistake, but it’s up there in terms of academic work.
John Marchica:
Yeah. Well, it is terrific. I want you to take me through the three areas or underlying causes as you say of our persistent poor performance. The first one is flawed assumptions. So, tell me about these flawed assumptions.
Dr. Elliott Fisher:
Sure. So, first, the people who do systems thinking, you’re probably quite familiar with how it’s being adopted by the CDC as a standard way of thinking about how to make health and healthcare better. Paul Osterman at MIT, Peter Senge, The Systems idea.
John Marchica:
Yeah, Fifth Discipline.
Dr. Elliott Fisher:
It’s understanding your own and other’s mental models if you’re trying to make sense of how to change things. I mean, I think one of this underlying cause that I think is very important is that not everyone, but many people in the public and among professional organizations, physicians, still hang on to a number of mental models, the way they think about what’s going on in healthcare, that constrain us or that are just plain wrong.
So, an example of plain wrong is health is produced by healthcare. More and more people are now recognizing, thanks to the tragedy of COVID-19, thanks to increasing attention to systemic racism and disparities, that health is produced by all sorts of things. It’s an old idea going back to Bob Evans and the determinants of health, but it’s gaining credibility.
What we know is that health has multiple determinants, social, economic, behavioral, and healthcare is one of those things, but in terms of the overall health of the population, healthcare is probably a relatively small fraction. So, we need to have a broader mental model that said health determinants include healthcare but others need to have attention paid to them.
The second one is, and I went to medical school thinking this was the case, the purpose of healthcare is to improve health and prolong life. I’m taught through my biomedical training all of the interventions I can undertake to make you live longer without seeing that that’s got some challenges. The purpose of healthcare is actually to help individuals achieve their own personal goals, one of which may be life extension, but toward the end of life, that shouldn’t be for many people that age is a priority and is outweighed by the quality of life that remains to them, but also much more or equally importantly is that in so many of the choices we make related to healthcare, patient’s values should be predominant. Their goals differ. Some people care about their symptoms and are terribly bothered by them. Others are not.
So, the whole acceptance in principle of shared decision making and the importance of engaging patients to make choices because there are always trade-offs among the conditions we’re treating, among the options for treatment. Classic examples, birth control for women, elective surgery for heart disease, they’re classic examples, and patient’s goal should drive care. So, I think that’s the second mental model people have, especially physicians and patients, “Oh, my doc should tell me what to do.”
We need to have patients engage in their decisions and that was the third flawed mental model that we had that patient should defer to their physicians when, no, wise decisions require both the physician’s and the patient’s expertise. Wise decisions require both of our knowledge, and treatments should be given to patients when they understand what the trade-offs are and can be helped to make or have the treatment recommended for them that’s best aligned with what they want to achieve.
John Marchica:
That was the first concept I think that I learned at Dartmouth, and it was entirely foreign to me. Isn’t that amazing? It makes so much sense. In fact, I spent a lot of time that first year when Hilary was my adviser. It was just such a foreign concept that I thought, but then once you learn it, it makes so much sense.
Dr. Elliott Fisher:
Yeah. It will be a real culture change, but this is, again, why haven’t we changed these things in the last 40 years when we’ve known this stuff for almost 40 years? It’s because these mental models are so deeply rooted.
John Marchica:
Right.
Dr. Elliott Fisher:
Another one that I think is probably as important, but unrecognized is most people think about medical care as a treatment or a diagnostic intervention. It’s the pill, it’s the device, the procedure that should be provided. Along with that is the rising cost or due to the rising cost of biomedicine. Yes, drugs are expensive, but the notion of biomedical interventions ignores this whole other piece, which is how healthcare is delivered. That’s increasingly recognized by advanced organizations and people who are trying to reform healthcare, but the question of how, where, how often, and by whom treatments are provided is critically important.
We’ve seen that with COVID, right? We were suddenly able to switch overnight to telemedicine. Well, what a wonderful thing for patients who live 50 miles away from their physician, but we’ve ignored that up to now. You can deliver great care. Often, nurses or community health workers can deliver much of what we need to deliver to people and it’s about who’s doing it, and in what way.
There are tremendous savings to be achieved and improvements in care from thinking more about how care is delivered. The innovations that could let patients get great care in much cheaper and better ways.
John Marchica:
I mentioned the study that we’re working on and my colleague asked me out of the blue the other day, “So, what’s the one thing that you’ve learned?” What one gem can I pass along? However marginal that I think that healthcare just got a little bit better, through all of these innovation, forced innovation, innovations in certainly telemedicine having to turn on a switch overnight, really, people using Zoom and whatever platform that they could get to provide healthcare service.
Other ways of better infection control, more efficient processes in the hospitals themselves. I haven’t quantified this in any way, but you know this just anecdotally from the things that you read about what’s been going on in the COVID era that they’ve been forced to innovate. So, do they have the right formula, right place, right care, right time? It’s like a lot of these health systems they have that as their motto.
So, all right. Back to the paper, so the second cause of poor performance is inadequate information or inadequate information systems. So, talk a little bit about that.
Dr. Elliott Fisher:
Yeah. It’s pretty remarkable that our financial system is able to update our credit reports every night based on where we shopped deeply fragmented pluralistic world. Yet, when I fill up at my physician or for my telehealth visit, he has no idea and has no access to my business to CVS, for my flu shot or to the visit I had out at the University of California in San Francisco what appeared to be a worrisome infection.
So, we’re operating even just if you think only about the information required to deliver great care to the patient in front of you. We have completely inadequate information. If you’ve gotten all of your care within Epic in a monopoly system that’s large and got Epic, you probably got most of that, but if you’re traveling in most of the country where people are still not on a single integrated healthcare system, just delivering good care isn’t there, but probably more, not more, there are all such deep problems, equally problematic, equally problematic is that we do not use the existing information to understand the risk and benefits of the treatments we’re receiving everyday, especially for subgroups of the population who may have different reactions. So, we do not have great data for African-Americans or for Native American populations about what maybe reasonable biologic differences in treatment, effectiveness in different subgroups or the elderly or children.
We assume that because treatments have been approved or used, that they are effective in everyone. We don’t understand their side effects or complications or whatever. So, the second area is understanding the effectiveness of common treatments or unusual treatments. I mean, this is a big country. If we had complete data on the outcomes of every treatment being tracked through the daily encounters of patients and physicians treating them, we could have precise estimates of the adverse outcomes associated with a given treatment and their costs, and be able to make much wiser choice back to this question of shared decision making.
So, we have lots of innovation in devices and in drugs, but they’re fundamentally evaluated superficially, devices, barely at all because they get grandfathered in if they are similar to some prior device, and drugs because there’s really not an expectation by the public or by the FDA that drugs should be compared to the other drugs that are available for that condition as opposed to placebo, so that we have lots of Me-too drugs that are better than placebo, but you can’t tell them apart.
So, that’s another area of lack of information. I think that the related area, so there’s the treatments themselves and what their outcomes are, but the related area is the quality of the providers that we’re going to see.
Anyone listening who wants to have nightmares for a little while should listen to the podcast Dr. Death about a neurosurgeon who was fellowship-trained, and then moved to Texas, and was totally incompetent. The fellowship hid how incompetent he was, and he was killing patients. It wasn’t our regulatory systems in the physician professional oversight that caught him. It was the police who busted him for murder because no one else was standing up.
That’s an outlier, but we know, when you look at John Birkmeyer’s work, there are two or threefold differences in both the technical ability of surgeons to do procedures, and then the ability to save people’s lives who’ve had a complication. Those are the two things that lead to bad outcomes in surgery. One is failure to rescue. That’s if someone has a complication and the hospital doesn’t figure out you’re septic or doing the procedure the wrong way or not knowing well-enough how to do it.
All of these problems of inadequate information on treatments and inadequate information on the quality of providers could easily be addressed with electronic. Now that we have the electronic connectivity and the technical tools to allow information to be pulled from across the healthcare system for a given patient, so that you can now give permission to an organization who could pull all of your information into a personal health record using APIs, these electronic ways of going [inaudible 00:24:40] I don’t understand it. I can’t even remember what it stands for, but it goes out into the net, finds the organizations, and pulls the clinical information, which has been standardized and can create a registry for you or by the system. So, better information is just so essential to this thing.
John Marchica:
Yeah. If you just ask a basic question if I have skin condition, if I have something that is concerning me about my throat or whatever the case may be, I don’t have a good mechanism to go find the right doc. I mean, I have my primary care doc, who I trust, and he has relationships, he’s a good doc, but there really isn’t any publicly available information to say or God forbid if I am diagnosed with something serious to know who’s the best doctor to go to, and do I have access to that doctor. I’m in this for a living. I’m on the net. I’m researching. I should be able to find, but for the average person, especially, it’s not easy to do.
Dr. Elliott Fisher:
I’m afraid we’re basing our, even when you and I informed consumers are trying to choose, we’re basing it pretty much on reputation. I mean, there’s starting to be some better data available. Kudos to the efforts to start to look at hospital quality and surgical outcomes, but it’s fundamentally limited and we should see it as, “Oh, that’s neat,” but let’s build on it. Let’s make it stronger so that patients can make wise choices.
John Marchica:
Yeah. Out here we have, and I don’t know if they have this in Vermont or in California, but it’s Top Docs. I think it’s Phoenix Magazine, and it’s basically a popularity contest.
Dr. Elliott Fisher:
Yeah, exactly.
John Marchica:
There’s no data.
Dr. Elliott Fisher:
Some of my favorite, some of the most fun we’ve had writing papers in the last 20 years was talking about America’s best hospitals, and then just showing how different they were on every measure that you could look at because the best hospitals are it’s a popularity contest. It’s reputation. It doesn’t have anything to do with the quality of their end of life care, for example.
John Marchica:
Sure. So, last area and then we’re going to get to solutions, but I want you to talk about this. You alluded to it before, this fragmented delivery payment insurance systems that cause issues with cost shifting and things like that. So, the third area of poor performance.
Dr. Elliott Fisher:
Yeah. It’s really interesting. Part of, I mean, we see the fragmentation in just the lack of information. We’ve touched on a couple of those places that fragmentation gets us in trouble, but the challenge of cost containment, which is really important. All the evidence would suggest where in the United States, we’re spending 50% more than our nearest competitors, and we’re not getting any better results for it. Maybe there are a few areas where we’re doing, but, generally, we’re not doing better.
When you look at estimates of wastes in the United States, we’re spending 30%. We’re probably wasting 30% of what we spend. According to a paper by Don Berwick or a more recent one, who’s the author of whom I’m blocking on the name, but the problem is that it is just too easy to shift costs or raise prices if someone tries to squeeze you.
There’s a wonderful article by Bob Evans, a health economist in Vancouver, who wrote an article called Tension, Compression, and Shear. It’s about the competition between society trying to control the costs to keep everybody inside the balloon, and providers, and in the providers you’d include the payers because of the insurance companies, they all do better and make more money if the balloon gets bigger.
Whether it’s in insurance systems or in delivery systems, it is too easy to shift costs to some place else or to raise prices. So, insurers do this by shifting risk, by saying, “Oh, I know. I’m going to be an association health plan and I’m going to offer skimpy benefits, and so I can then all get to take care of relatively healthy people or when they get sick, I won’t have to pay for their cost.” That just means the cost when those people get sick are shifted some place else.
So, our insurance system is designed and the place that everyone’s enjoying shifting cost to, it’s a quiz. Who’s everyone enjoying shifting cost to?
John Marchica:
All of us. I’m not exactly sure how to answer that.
Dr. Elliott Fisher:
Yeah. Exactly. How’s deductible and copayments going?
John Marchica:
Not well.
Dr. Elliott Fisher:
We’ve had this huge increase in high deductible health plans, coinsurance, copayments. The burden of cost that is born by consumers has increased dramatically. Well, has it slowed the growth of healthcare cost one width?
John Marchica:
Of course not.
Dr. Elliott Fisher:
No. Once you’re sick, you’re not influenced by any of that. Copayments aren’t going to change your decision to be transferred to the ICU or not, and all the money in healthcare is spent on people who are sick. So, that piece can keep growing even as we shift more and more cost to consumers, which may save insurers a little bit. So, that’s one example of how costs can be shifted.
I think the more unfortunate one is it happens in the delivery system as well. We touched on this earlier with ACOs, right? So, ACOs are great. I was puzzled and now I’ve confirmed in conversations with all sorts of people who run these things that, but not all of them, we have our ACO for our Medicare population, right? We’re keeping them out of the hospital quite effectively.
We’ve reduced admissions and readmissions, and we’ve freed up those hospital beds and operating rooms for private pay patients who pay us much more than the Medicare patients. So, total healthcare costs aren’t touched by the ACO model right now. I am sounding skeptical like an old guy, and I’m sorry for the postviral cough, non-COVID as far as we know.
So, I think the capacity of the healthcare system to shift costs to others means that growth continues in inexorably. Growth and spending continues inexorably. Some providers also have the opportunity to raise prices if they happen to be a monopoly. So, they can get away with raising prices or by increasing the volume of unnecessary or discretionary treatments, said the healthcare skeptic.
John Marchica:
I love the concept of the balloon, right? Squeeze here. First of all, everybody wants the balloon to get bigger, but just because you’re collapsing here, the money goes out, goes over here.
Dr. Elliott Fisher:
Exactly. If I knew how to share my screen effectively, I could show you a picture, but we could try that. That would be exciting.
John Marchica:
Yeah. Absolutely.
Dr. Elliott Fisher:
Let’s see if I can get this to be a bit bigger. This is a radical idea. All right. Then go share screen my desktop. So, can you see that picture?
John Marchica:
Yes, I can.
Dr. Elliott Fisher:
This is the fundamental notion. There are lots of ways in blue that we can attempt to control cost. Public payers control their prices, bundled payments, ACOs, limiting the profitability of health plans by the amount they must spend on healthcare, increasing copayments, but the problem is all of those have comparable ways of shifting the cost and continuing the expansion of the balloon, raising prices, shifting cost out of the bundle. I mean, this is the tragedy of bundled payments. Using the ACO model to free up resources for higher paying patients, ugh. This is an embarrassment.
Mark and I created a way for people to make more money in healthcare. Raising premiums or offer low value plans that increase discretionary care for those who’ve met the deductible. Those are tragic. I’ll stop sharing now if I can figure out how to do that, so we can see each other again. There we go.
John Marchica:
Yeah. That’s very, very clear. So, given all of that, what is the solution? I guess to start off, I think you’re going to want to tell me what a population health organization is, but-
Dr. Elliott Fisher:
Well, yeah. Sure. I mean, I think we talked already about the challenge of ACOs and that they’re only for a narrow segment of the population, and that their in mixed payment models, right? So, I chose the term population health organization in this paper and I’m not sure now. I’m now regretting it, so maybe it’s not too bad that it’s hiding behind the paywall because it should have been advanced ACOs, right? I really do want to help ACOs be part of the solution here in the long run, and why would you throw away that name? It was a good name. Anyway, another topic.
John Marchica:
So, branding exercise, that’s part of it. You know I got, but it’s part of it.
Dr. Elliott Fisher:
I know. Anyway, but the notion is we need organizations who will be responsible for the health and total cost of care for the people they serve, and have a payment model that allows them to really takes full advantage of this payment model. That really has to be enrollment of a defined population under capitation, so that this primary care focused organization, provider organization can be rewarded for improving health, total health, keeping us from smoking, helping us, and reducing the cost of care.
So, it’s a focus on population health. It’s still the notion of a provider organization, very much like ACOs, but it’s saying, “ACOs, if you want to play in this, you should be committed to the model and shift to global payment for all your patients.”
That’s what starts to what is intended to start changing the dynamic within the organizations so they can now go really turbo charge their innovation, develop new teams, delivery great care. Some ACOs are doing this and they’re probably the prototype organization, but they got to get out of fee-for-service. We got to get them out of fee-for-service, so they don’t have the mixed payment model. So, maybe advanced ACOs would have been a better term.
John Marchica:
Maybe for the next paper.
Dr. Elliott Fisher:
Yeah, when I write something that someone will read.
John Marchica:
That someone will read. So, the single system, I want you to explain this how this all works and then what I want to do, and I realized we’re bumping up against some time, but I want to take that application and say, “Okay. Well, how would you do that in Massachusetts given that you have multiple integrated health system? You’ve got multiple large insurance systems or insurance payers, Blue Cross Blue Shield Massachusetts, Tufts Health Plan. You’ve got home health. You’ve got all of these different delivery mechanisms, as well as payment mechanisms? How would you actually implement something like this in a state?”
I just pick Massachusetts not so much at random because in many ways they’ve been down a certain path with their Romney Care and there’s some academic institutions there that are pretty well-known and esteemed, whether they deserve it or not, I don’t know.
Dr. Elliott Fisher:
Yeah. No. So, I think it’s a modest modification of our current scheme. First, on the delivery system side. Actually, let me start on the “payer” side. What I think we would all like and best benefit from is really good choices about what population health organization is going to take responsibility, where we’re going to throw our lot in with and they’ll take responsibility for us.
These should be provider organizations, which are rooted in primary care. So, they have strong primary care foundation and I like the idea of being able to have them compete, but be of different types.
So, maybe I’ll go back and show you a figure. Shall we share screen and I’ll show you a slide. How many hours spent on one figure that looks more confusing than people would really like to have to live with, but let’s go there. Oops, I got to share. All right. Can you see this image here? They can probably see us both. You just had a drink-
John Marchica:
Yes.
Dr. Elliott Fisher:
So, let’s look at this middle group here, which I refer to as population health organizations. The idea was the integrated delivery systems could be a population health organization. Consumers would get to choose these on a statewide exchange. That’s the notion. So, they could choose an integrated delivery system. That would be partners or Beth Israel Deaconess or a physician, a multi-specialty group practice that doesn’t own any hospitals. We’ve seen that the physician-led ACOs who’ve done better at reducing costs and those that have hospitals.
It could be just a primary care network. I believe there will be emerging all sorts. Can you see my mouse there?
John Marchica:
Yes.
Dr. Elliott Fisher:
There will be all sorts of emerging innovative practices, which could be rooted in telehealth and maybe local primary care practices or urgent care, but each of these for our prototypes to be capitated and responsible for keeping you healthy in all of your care. Some of these would as in at partners, all of your care could be delivered within that integrated delivery system. That would also be Kaiser Permanente in out west. Multi-specialty group practices would have to contract with a hospital to go when your patients are admitted.
Primary care practices might send to independent specialty practices or up to other specialty practices, but the notion is to have them competing on a level playing field to deliver the best possible care to all of their patients.
To make this work and I’ll come back in a second to why I think we need universal health insurance and Medicaid should just pay for enrollment in these things at the same way because the level of playing field starts to really have some benefits in terms of population health and inclusion, but you’d have a regional or statewide insurance exchanges, PHOs or let’s say advanced ACOs would offer health plans almost certainly in partnership with a payer, but you’d probably like to have the alignment be pretty one payer would give a primary payer and the other payers if referrals would work with them.
I think this is where you get competition on overall cost and quality as consumers make annual choices of population health organization. It is essentially trying to bring to fruition what Alain Enthoven suggested [inaudible 00:43:12] 40 years ago as managed competition rooted more in provider organizations than in payers because no one knows what the network is the physicians you’re signing up for.
Whereas if you talked about Atrius or Kaiser or Mass General, you would know who you were talking about getting care from. You’d be able to look at the quality of the providers.
The other piece that I advocate is this competition on cost and quality for condition and episode-specific care. This is about the better information. Imagine if everyone, whether you’re a Kaiser or a Mass General had to report condition-specific quality and cost with meaningful outcomes, then if you were getting your joint replacement at MGH and the validated data said, “Well, this outpatient specialty practice over here has much better outcomes,” either Mass General would have to improve to persuade you to stay in or you’d have a pretty good argument for going outside. We’d start to learn how to deliver great condition-specific care because we have the examples of the outstanding providers from which everybody could learn. So, that’s the basic notion.
John Marchica:
So, if I am just trying to nail this down, it’s happening here in Arizona, these advanced ACOs, they’re on an exchange. Is this still tied to employers? In other words, would I be offering a choice of advanced ACOs to my employees and then they would make a decision?
Dr. Elliott Fisher:
I hope so. The more we are a single system, the less we’ll have the pricing disparities, which make it easier for employer-based plans to be cheaper than individual plans. There’d be risk adjustment or missed equalization to make the payment system work, but you want competition on a level playing field.
So, I would ideally have employers once they see that the exchanges offer better value to them than trying to create something themselves, they would want their employees, and employees would want to be part of the exchange with transparent competition on quality and price.
John Marchica:
What’s really interesting about this is your conscious avoidance of the term single payer, right? It’s a single system, which could be a single payer or it could be multiple payers, which is the way that this chart is lined up. You’re given two different choices. Is that because the single payer, from a political standpoint, is one of those hot buttons for some people?
Dr. Elliott Fisher:
I think it can be a hot button for some people. Single system, by the way, is going to be a hot button for others, right? Everyone’s terrified at being in a single system. This is another branding challenge. You can help. Maybe it should have been a better choice.
Dr. Elliott Fisher:
So, fostering better choices for Americans, the better choice plan, but single payer, I wanted to be prepared to try to say regardless of what you think about coverage, whether it’s single payer or multi-payer or repeal and replace, the underlying problems in the healthcare system, the high cost, lousy quality or not as good quality as we could have need to be address. That’s about better information, and meaningful competition at every possible level, making the market work for treatments, for choices of providers, and for choices of plans. If you have good information, then the market can work to really drive value.
John Marchica:
Right, right.
Dr. Elliott Fisher:
Because right now, right now, competition is about avoiding risks and shifting costs. How can you play the game to make more money yourself rather than competing on value?
John Marchica:
So, we’re recording this not sure when this will air, but we’re recording this in the aftermath of the election. I’m wondering what your thoughts are. Well, let me back up. With the last administration, I was very concerned that a lot of the progress that had been made, the Affordable Care Act was in jeopardy and in some ways, it has been. In other ways, ACOs, bundles, the CMS is pretty much so kept on track. There’s been a few things that they’ve made modifications to.
So, now as we’re in Biden era, what do you see transpiring, and let’s make the assumption. Again, we don’t know this. Let’s make the assumption that it’s a Republican health senate, so the political side of things. What’s going to take place in healthcare delivery reform, we’ll say payment and delivery reform over the next couple of years? What do you think will be happening?
Dr. Elliott Fisher:
Well, of course, prediction is really tough, especially about the future. So, I think that was Niels Bohr, in fact. It’s like, “Hmm.” So, it’s hard to predict. I think we can look back and say there’s broader agreement on the right and the left that moving toward value-based payment, toward paying in ways that reward better care and lower costs is accepted wisdom.
There’s resistance to it, but I think it’s accepted wisdom that that’s the way we should go. I think there’s some misunderstanding about whether the more fragmented approach like bundled payments is sufficient, and that’s why I advocated for capitation as a wraparound within which the bundled payments, you could know that they’re driving better value overall by reducing the cost for the populations cared for in each advanced ACO or PHO.
So, I think value-based payment is here to stay. I think there will be a lot of experimentation at the state level in how to move this forward faster. I think I’m hopeful that CMS will continue to offer through CMMI new incentives to expand and strengthen advanced alternative payment models, especially those related to global payment.
I think that the barriers are employers. ERISA gives them an out to not have to play along with everybody else, which makes state action harder, but I’m curious, and I’m now starting to try to learn a little bit more about it, but don’t have an answer yet. What can states do to encourage employers and private payers to move toward a global payment model with their providers, in partnership with providers? I think that’s where I see the future being able to deliver on the promise of accountable care.
John Marchica:
Last question. Is the state of Maryland a good place to try to implement what you’ve been talking about?
Dr. Elliott Fisher:
I think Maryland might be a promising place. They’ve got the waiver that lets them do global payment models. I think Massachusetts. I look to the states that are at the forefront of efforts to move forward. I think California, it’s big, but it’s got a very progressive agenda, and I know there’s strong interest in both strengthening measurement at the provider level within independent healthcare association and the public payers are very interested in trying to move toward integrated care models because they see the difference between the quality of care that’s achieved by Kaiser Permanente in California compared to the more fragmented systems, Kaiser Permanente in particular. Sharp is also strong, but they’re 30 percentage points better on most quality measures than the fragmented fee-for-service system. That’s a big difference.
John Marchica:
Yeah, and you’d find something similar, Geisinger or Intermountain, when they have this tight models, tightly integrated models.
Dr. Elliott Fisher:
Yeah. Why don’t we reward them and get everybody to play the same game? I do want to just a word about this moment in American history where systemic racism and the impact of disparities in access in care for disadvantaged populations have been driven home so powerfully by COVID-19. The other, I think, one of the strengths of this notion of getting us into a single system that I didn’t mention earlier is that by creating a single system, it is by definition inclusion.
If you are poor and in a town where everyone’s lost their employment or the major employers left or if you are Black and have no opportunities in the devastated community where you’re living, being relegated to the safety net is by definition makes you feel less, makes you feel less part of the country, less part of the community.
One of the things I really hoped for with this model was to say, “Hey, it could be that this is a step toward the inclusive society that we really believe is important while staying totally aligned with the principles of the market and competition.”
My colleagues at AEI or elsewhere or Heritage would say, “Those are the principles that we believe in.” If we could get them to see that you can’t have competition in a market that doesn’t have a level playing field, that are regulated playing field or regulated system, enables you to make the market work. It could be better.
John Marchica:
It could be. The thing that’s disconcerting is that the ACA tried to do that, tried to implement all of these really market-based reforms and it became this political Obama Care, we’re going to try to get rid of it how many times? 57 times? I don’t know even know what the last count was of trying to-
Dr. Elliott Fisher:
I think the hearing is today, right?
John Marchica:
Right.
Dr. Elliott Fisher:
Supreme Court is hearing arguments today.
John Marchica:
So, it’s just unfortunate that sometimes people, they just don’t want to hear it, but that doesn’t mean that we don’t fight the good fight, and that you don’t do the work that you do. Elliott, this is terrific, terrific paper. I highly recommend it to our audience. Pay the five bucks or 10 bucks or whatever it is that they’re asking for it.
Dr. Elliott Fisher:
I wish.
John Marchica:
Oh, is it more than that?
Dr. Elliott Fisher:
Selling a journal is not cheap, right?
John Marchica:
Right.
Dr. Elliott Fisher:
I had the longest fight with them about this thing. Whew.
John Marchica:
Well, the next iteration then that, no matter what, I still highly recommend it.
Dr. Elliott Fisher:
If people want to use it for teaching purposes, they should email me-
John Marchica:
I will be doing that.
Dr. Elliott Fisher:
… or people who are listening to this.
John Marchica:
Yeah, or other people, but I’ll be doing that.
Dr. Elliott Fisher:
If it’s for educational purposes, I believe the copyright laws allow me to share it.
John Marchica:
Terrific. Well, I hate for this to end. Elliott, this has been terrific. I’ve enjoyed every minute of it.
Dr. Elliott Fisher:
Me, too.
John Marchica:
Just make sure to keep in touch. I appreciate your spending so much time with me, really.
Dr. Elliott Fisher:
Well, it’s a fun conversation. Thanks for reading the paper. Thanks for giving me a chance to talk. You know I love to talk.
John Marchica:
All righty.
Dr. Elliott Fisher:
Take care.
John Marchica:
Thanks. Take care.
Kim Asciutto:
From all of us at Darwin Research Group, thanks for listening. Health Care Rounds is produced by me, Kim Asciutto and is engineered by Andrew Rojek. Theme music by John Marchica. Darwin Research Group provides advanced market intelligence and in-depth customer insights to health care executives. Our strategic focus is on healthcare delivery systems and the global shift toward value based care. Find us at darwinresearch.com. See you next round!
About Darwin Research Group
 Darwin Research Group Inc. provides advanced market intelligence and in-depth customer insights to health care executives, with a strategic focus on health care delivery systems and the global shift toward value-based care. Darwin’s client list includes forward-thinking biopharmaceutical and medical device companies, as well as health care providers, private equity, and venture capital firms. The company was founded in 2010 as Darwin Advisory Partners, LLC and is headquartered in Scottsdale, Ariz. with a satellite office in Princeton, N.J.
Darwin Research Group Inc. provides advanced market intelligence and in-depth customer insights to health care executives, with a strategic focus on health care delivery systems and the global shift toward value-based care. Darwin’s client list includes forward-thinking biopharmaceutical and medical device companies, as well as health care providers, private equity, and venture capital firms. The company was founded in 2010 as Darwin Advisory Partners, LLC and is headquartered in Scottsdale, Ariz. with a satellite office in Princeton, N.J.
Contact Darwin Research Group and we will get right back to you.
Reach out to us
Gainey Corporate Center
8777 N Gainey Center Dr, Ste 205
Scottsdale, AZ 85258
(480) 923-0802

